What is long covid post-viral immune dysfunction?
The aftermath of COVID has been widespread and has impacted us all at many levels physically, emotionally, spiritually and mentally. Many of us have known someone who has died from COVID or are experiencing the long-term consequences of the virus.
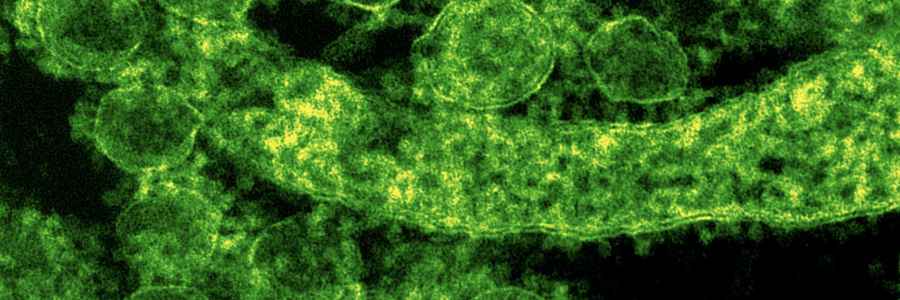
The concept of post-viral syndrome is not new. Some people can develop this phenomenon after a cold or bout of flu. Long COVID occurs when signs and symptoms persist after the acute infection phase. It is possible to experience symptoms for six months or more.
Who is more at risk for long COVID?
It is hard to predict who is at risk for developing long COVID. Some studies have shown no relationship between severity of the virus, others have suggested age, sex, hospitalisation and asthma are factors in susceptibility to post-virus symptoms. Other considerations include persistent virus within the bloodstream because of lowered or absent antibody response, reactivation of other viruses, inflammatory and immune reactions, poor gut health or poor circulation.
What are the common symptoms of post-viral infection?
Certain diseases and chronic fatigue syndrome (CFS) are linked to long-term viral side effects. The initial acute symptoms vary but the post-infection repercussions seem to be surprisingly similar. These include fatigue, neurological problems, muscle and joint pain, trouble sleeping and irritability. Studies show that 80% of long COVID sufferers will experience fatigue. Other symptoms of long COVID include shortness of breath, coughing, chest pain, loss of taste and smell, digestive symptoms, memory loss, brain fog, anxiety and depression.
Even though COVID can be viewed as a viral respiratory disease, it has the potential to affect multiple organs. Data has shown inflammation and immune system imbalances continue for at least eight months after the initial infection. Fatigue is a common central symptom. The approach is to manage and conserve energy levels, similar to CFS.
Researchers at Otago University are also linking long COVID to brain inflammation that exhibits side effects similar to patients with CFS. Unfortunately, how these brain effects develop is not well understood. This was what they had to say…
“This work highlighted that there is a susceptible subset of people who develop such syndromes when exposed to a severe stress, like infection with COVID-19, or the glandular fever virus Epstein Barr, or in some people with vaccination that is interpreted as a severe stress.”
A transient infection becomes chronic and the disease persists.
How can we as Health Practitioners help?
Immune support is central to healing. Vitamin A, C, D and zinc are essential for immune function. Recent data has suggested that those with long COVID have lower levels of vitamin D.

Vitamin D mainly comes from spending time in the sun but many of us don’t get our recommended daily exposure. By eating six to eight eggs a week you can get the vitamin D you need. See the yummy Jamie Oliver recipe in our recipe section. Other foods that contain vitamin D are oily fish (salmon, herring, mackerel and sardines) and mushrooms. Browning mushrooms in the sun can increase their vitamin D content. If you are vegan, a good D3 supplement would do the trick.
Aim to eat up to three and a half cups of vegetables daily, particularly leafy greens and up to two portions of fruit daily. For nutrient density, the more colourful vegetables you include on the menu, the better. Zinc is found in fish, red meat, pumpkin and sunflower seeds, whole grains, beans, nuts (pecan, Brazil, almond and walnuts), organic tofu, miso, mushrooms and green beans.
Since 80% of our immune system is found in the gut, it is important to ensure that things are working well in this department. Choosing organic foods and personal care products, where possible, lowers the risk of putting a further burden on the system by exposure to pesticides and other toxins. Exercise is essential for the function of all physiological systems; the key is finding a good balance of exercise intensity.
Summary
Managing any post-virus syndrome is complex and challenging. Strengthening the immune system is central to restoring health. Progress may be slow and a great deal of patience is required. Small sustainable changes over time are a sensible approach and having a trained practitioner guide you can be hugely supportive. Sleep, balanced meals, appropriate exercise, rest and being kind to yourself will go a long way in helping your recovery.
References
Leech B. (n.d.) The Nutritional Qualities of Eggs, a brief review. https://files.constantcontact.com/65807bf2201/f554d22c-9824-40ad-97bc-88ca8d34420c.pdf?
Jamie Oliver. (2023). Potato, pepper & broccoli frittata. https://www.jamieoliver.com/recipes/vegetable-recipes/potato-pepper-and-broccoli-frittata/
Owen B. (2022). How “long covid” is shedding light on post-viral syndromes. https://www.bmj.com/content/378/bmj.o2188#
Campos, M. C., Nery, T., Starke, A. C., de Bem Alves, A. C., Speck, A. E., & Aguiar, A. S. (2022) Post-viral fatigue in Covid-19: A review of symptom assessment methods, mental, cognitive, and physical impairment. Neuroscience and Biobehavioural Reviews, 142. https://doi.org/10.1016%2Fj.neubiorev.2022.104902
BioMedica Nutraceuticals. (2022, July). Research Update: Addressing the long COVID crisis with natural medicines. https://www.biomedica.com.au/media/contentmanager/content/Addressing
_the_Long_COVID_crisis.pdf?
Tate, W., Walker, M., Sweetman, E., Helliwell, A., Peppercorn, K., Edgar, C., Blair, A., Chatterjee, A. (2022). Molecular Mechanisms of Neuroinflammation in ME/CFS and Long COVID to Sustain Disease and Promote Relapses, Frontiers in Neurology, 13. https://www.frontiersin.org/articles/10.3389/fneur.2022.877772/full
Busko, M. (2023, May 16). Could Vitamin D Supplementation Help in Long COVID. https://www.medscape.com/viewarticle/992013