Are you Listening to your Gut?
COVID-19 has brought home to me just how fast things can change and how important our health is.
We have been well-advised on how to limit our exposure to the virus through hand washing and social distancing. Another hugely important step you can take, is to strengthen your immune system.
And that begins in the gut! Did you know that up to 80% of your immune cells are located in your gut?
It is becoming more evident and more widely accepted that immunity and the gut microbiome are linked. So what is the gut microbiome?
It’s a community of trillions of living microorganisms, mainly bacteria but also viruses, fungi and other microbes. You have developed a mutually beneficial relationship with your microbes that function together as an ecosystem. An imbalanced ecosystem, also known as dysbiosis, can cause a number of problems including brain fog, mood issues, weight gain, diabetes and autoimmune conditions.
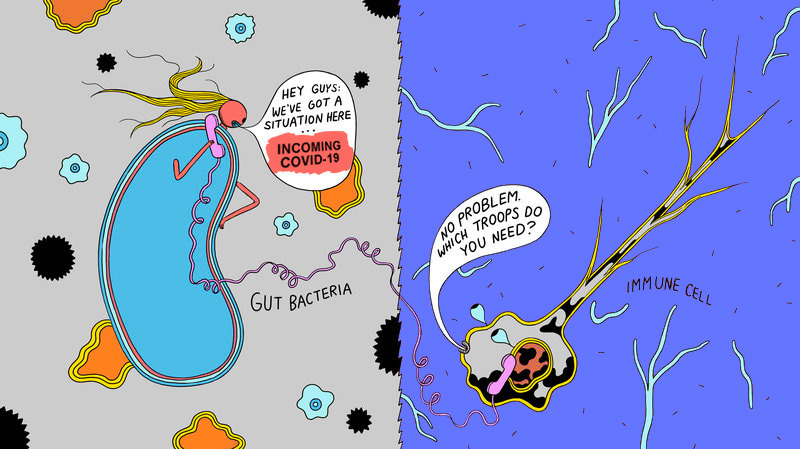
Your gut microbiome has its own language and bacteria communicate with each other independently.
When you eat a meal, your bacteria will have a biochemical ‘conversation’ about it and decide where those nutrients are most needed. Your bacteria are able to sense how stressed, how happy, how anxious or angry you feel. They are also able to influence your emotions by generating and modulating the signals that the gut sends back to the brain. I find it fascinating that what you eat can affect your mood!
The immune system is your own personal army, made up of cells and molecules that protect you from disease. It continuously monitors your body for foreign substances. Your immune system has developed alongside the gut microbiome, they work together to keep you healthy and protect you from those ‘bad’ microbes.
The dialogue between your immune system and the gut microbiome begins at birth. When things are functioning well, the immune system promotes the growth of the good bacteria and keeps things in balance. The microbiome supports the development of immune cells and helps with fine tuning immune responses.
How the immune system works
Reiki is a vibrational or subtle energy therapy that uses light touch to balance
The immune system has two types of responses – innate (born with) and adaptive (acquired). Your innate immunity is your first line of defense. It is made up of physical components (skin, gastrointestinal tract, respiratory tract and body and facial hair), chemical barriers and cells that patrol your body looking for threats from ‘bad’ microbes. The main purpose of the innate immune response is to destroy foreign, damaged or infected cells immediately, preventing the spread of the foreign microbes throughout the body.
If the threat becomes more that the innate immunity can deal with, the adaptive immune system kicks in. This system has the ability to remember past infections and vaccines and is quick to respond when it recognises something similar. Adaptive immunity is mediated by cells called lymphocytes, which are made up of B and T cells.
B cells produce antibodies to neutralise the problematic microbes. Antibodies in the blood and gut secretions recognise microbial antigens. Antigens are anything that causes an immune response. They can be either bacteria, viruses, fungi, parasites or proteins that pathogens secrete. Look at them as name tags. A general antigen will announce to your immune system, “I’m dangerous.” A specific antigen will announce, “I’m a bacterium that will cause an infection in your gut.”
In the future it might say, “I’m the coronavirus and I’m going to give you pneumonia.”
T cells don’t secrete antibodies, they release cytokines, which are molecules that are used for cell to cell communication. Cytokines are involved in many aspects of inflammation and immunity. Certain cytokines trigger the familiar symptoms of fever, inflammation and pain, when your body is fighting an infection.
What irritates your protective wall?
Alcohol is a gut irritant, which causes inflammation and damages the digestive tract. Many wine and beer drinkers have sensitivities to yeast and sulphites. Alcohol also doesn’t play nicely with your gut microbiome. It changes its composition. This has been implicated in cancer.
Antibiotics do not discriminate between health promoting and ‘bad’ bacteria. The destruction of the microbiome causes inflammation and can lead to ‘leaky’ gut. In some cases, antibiotics are absolutely crucial, but they shouldn’t be used indiscriminately. My advice is to use a good probiotic during and following antibiotic treatment.
Painkillers, particularly non-steroidal anti-inflammatory drugs (NSAIDs) are not great for your digestive system. NSAIDs increase the likelihood of ‘leaky gut’. Paracetamol doesn’t have the same effect on your digestive system, but it does overload your liver.
Coffee and tea irritate your gut lining and prevent the absorption of important minerals. The odd cup of coffee or tea is unlikely to be a problem, but if you have digestive problems, they probably aren’t your best friends.
Deficiencies in cell-building nutrients such as vitamin A, zinc, glutamine and essential fatty acids (EFAs) can cause poor gut wall structure. An overgrowth of the wrong bacteria or fungi or other parasites, can burrow into the intestinal wall causing ‘leaky gut’.
Overeating can also stress the gut wall. When your body is having to deal with extra toxins, your liver will be working at full capacity.
Take Home Message
The health of your microbiome depends on what you eat and drink. They break down food into thousands of metabolites, which impacts your gut, including the nerves and immune cells. These metabolites enter the blood for long distance signalling and can affect every organ including the brain.
If you have gut symptoms of constipation, diarrhoea, bloating, pain or have skin issues, arthritis, fatigue, mood disorders, inflammatory bowel disease, your gut is trying to tell you something!
It’s not all doom and gloom. The good news is that with a good diet, lifestyle and the right supplements, you can improve your gut health. The key will be to remove the irritants and any foods that you are sensitive to. Identify any gut infections from rogue microbes and treat them. This is followed by re-inoculating with good bacteria and healing your gut. It is a process that would need professional guidance.






